Psychedelic Science & Neurochemistry
Anyone familiar with the psychedelic space has likely heard stories of these substances’ transformative potential. From the hundreds of clinical trials showing the efficacy of psychedelics in the treatment of depression, anxiety, PTSD, addiction, and beyond —to reddits, Erowid trip reports, Tim Ferris podcasts, Michael Pollan’s “How to Change Your Mind” and Paul Stamet’s “Fantastic Fungi” – The powerful healing potential of these compounds has officially become established within the mainstream consciousness.
The overwhelming evidence suggests that when psychedelics are used with mindful intention, within an integral & safe container, and followed up with a compassionate integration process – they can bring about unprecedented rapid shifts in personal growth to both individuals and collectives. Yet how these plant compounds have such a profound impact on the human psyche from a neurological perspective has only recently received the focus & support necessary to explore in great detail.
We are living within a frontier, a time of exploration and discovery unprecedented in the age of modern medicine. Where psychedelics are opening a door toward shifting the mental health conversation not experienced since the introduction of Prozac & the creation of SSRIs 30 years ago. Yet just how prolific is psychedelic research at this time? We often forget or dare I say are conveniently uninformed, of a 15-year period beginning in 1950 where research on LSD and other hallucinogens generated over 1,000 scientific papers, several dozen books, and six international conferences – along with being legally prescribed as treatment to over 40,000 patients.
Since Jon Hopkins University’s 2007 landmark study on the meaningful mystical significance of psilocybin effectively broke the gauntlet on Nixon’s 50 year Drug War (AKA War on Race & Consciousness), 309 universities have taken up the torch of conducting psychedelic clinical research trials. Meanwhile, 24 phase II trials (and in one case MAPS MDMA completing a phase III trial) have been completed by non-profits and research organizations on the efficacy of LSD, DMT, MDMA, Psilocybin, and other classic & novel compounds.
Serotonin & Neuroplasticity
Like psilocybin and DMT, serotonin is a tryptamine—an organic molecule (or indole) that shows up throughout the natural world. As dopamine can be considered the “give me more” chemical, serotonin on the other hand, is the “I am enough, I have enough, I am content” neurotransmitter.
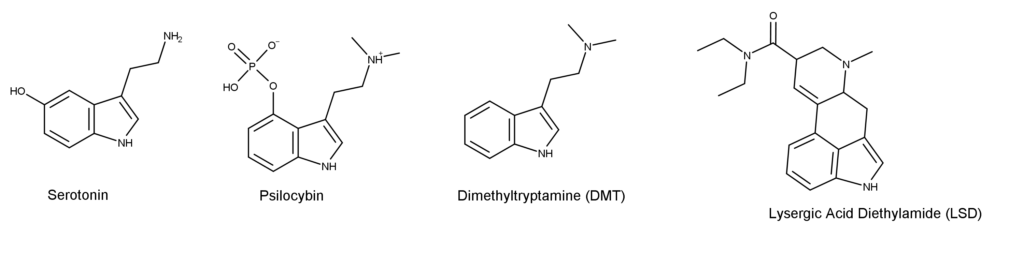
While psychedelics do not work like SSRIs modulating the reuptake of serotonin in the brain increasing its availability, they do stimulate a particular serotonin receptor called 5-HT2A—or serotonin 2A. In fact, LSD binds to the 5-HT2A receptor even more than serotonin does, which may explain why LSD experiences last as long as they do.
While 5-HT2A receptors are found throughout the body, including within the digestive tract,, they’re especially prevalent within the prefrontal cortex—the area of the brain responsible for complex cognitive behavior, personality expression, decision-making, and processing information from all other brain systems. In this context, stimulation of the 5-HT2A receptor leads to (among other things) two significant results:
The first being the production of brain-derived neurotrophic factor (BDNF), a protein that nurtures existing neurons and promotes the genesis of new ones. This process of increased connectivity between neurons is called “dendritic sprouting”. A key component of neuroplasticity or the brain’s ability to modify, change and adapt in both structure and function throughout life and in response to experiences.
The second is the Increased transmission of glutamate, the neurotransmitter most responsible for brain functions like cognition, learning, and memory; which also plays an essential role in promoting neuroplasticity. One way it does so is by improving connectivity between the prefrontal cortex and the hippocampus—which also contributes to the growth of new dendrites. Increased levels of glutamate in the medial prefrontal cortex also seem to trigger the state called “ego dissolution”, during which people temporarily lose their sense of self or isolation and instead experience a sense of oneness and unity.
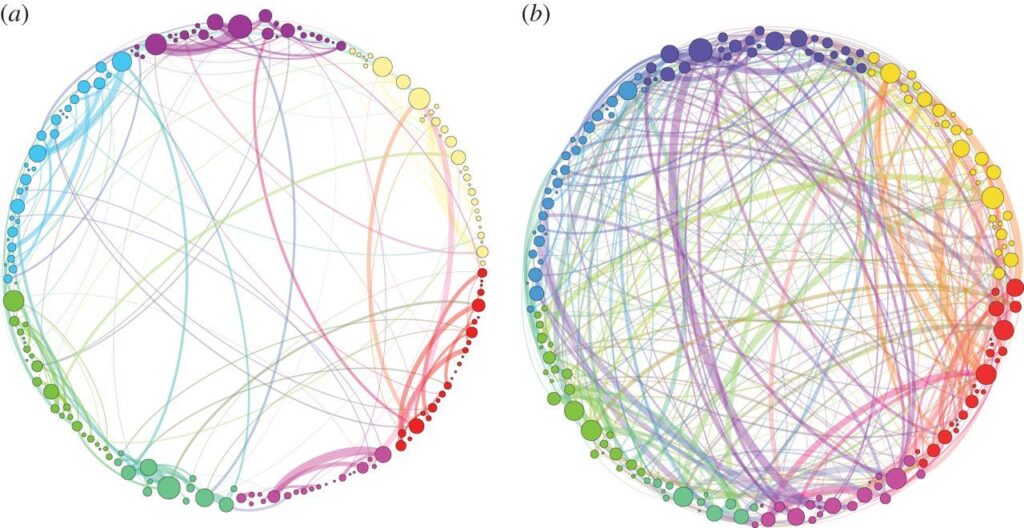
Psychedelics’ capacity to link otherwise-disconnected brain regions was beautifully displayed in a 2014 research article called “Homological scaffolds of functional brain networks”. A simplified illustration showed the neural connectivity patterns of a brain on psilocybin compared to a research subject given a placebo (see image below). This interconnectivity is likely responsible for the hallucinations and synesthesia often experienced by psychedelic users Additionally it can be the main contributor to lateral and divergent thinking, learning new patterns, experiencing novel visionary insight, and even anamnesis with both high dose & prolonged microdose psychedelic experience.
Default Mode Network (DMN)
Psychedelics have also been found to decrease blood flow to the brain’s default mode network (DMN), the part of the brain that is active when people aren’t engaged in any particular project or activity.
An active DMN is essential to helping us filter out the “noise” associated with daily life. Without it, we would likely become overwhelmed by the sights, sounds, smells, and sensations that come at us on a constant basis. It is essentially the brain’s efficient & effective filter operates. However, an overactive DMN may result in excessive rumination, repetitive thought-loops, and ‘paralysis by analysis’—all hallmarks of conditions such as obsessive-compulsive disorder (OCD), addiction, anxiety, and depression.
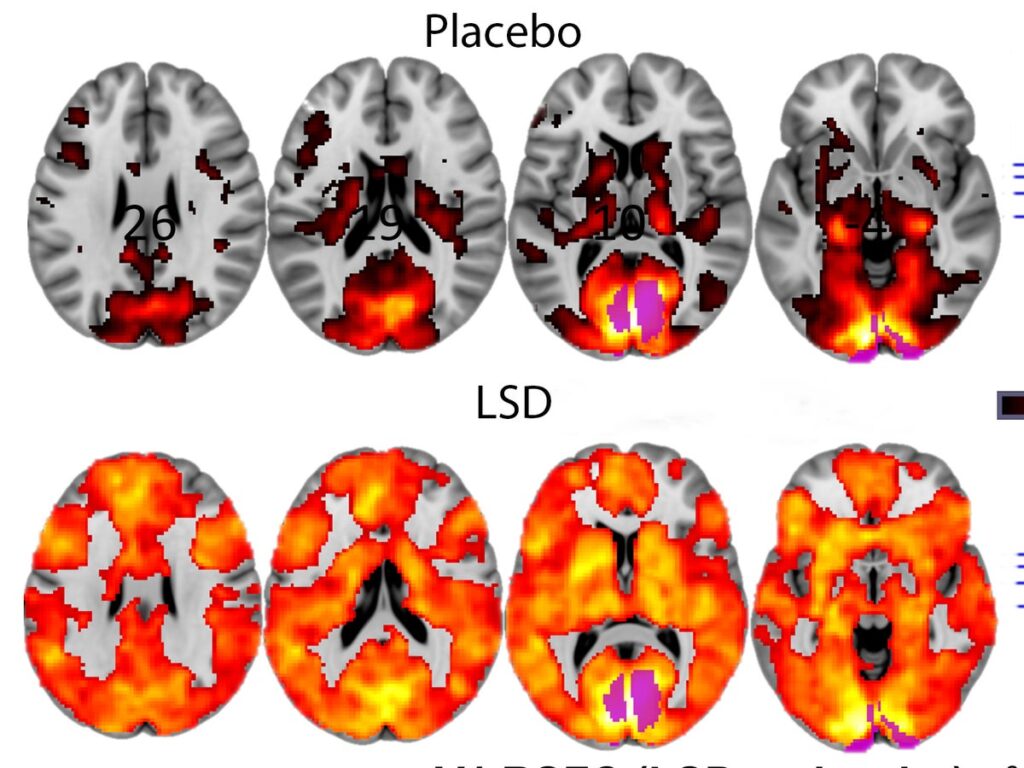
By quieting down the DMN, psychedelics such as ketamine, psilocybin, and LSD allow people to become more grounded in the present moment, achieving a state of mindfulness that may enable them to better observe their deepest thoughts and emotions without becoming attached to them. Allowing for forgiveness, nonattachment, acceptance, and genuine resolution. Interestingly, a similar state is observed among experienced meditators.
Sympathetic vs Parasympathetic State
In addition to disrupting the DMN, psychedelics also decrease activity in both the amygdala and anterior cingulate cortex—areas of the brain associated with fear, negative emotion, and depression. This may explain their efficacy in helping to treat anxiety, depression, and PTSD. When constricted, the amygdala sends the body into a sympathetic or survival-minded state. When triggered, it results in a release of epinephrine, corticotropin, and cortisol—hormones designed to help us counter situations of physical danger. If it becomes overactive, however, hyperglycemia, hypertension, and cardiovascular disease can result. Sympathetic system dysfunction has also been tied to mental health conditions such as anxiety, depression, and chronic stress. When suspended in the fight, flight, freeze, or fawn – people are more likely to experience adrenal fatigue—hampering the body’s natural ability to self-repair. Yet this highly anxious, tense, reactive state is not from running from lions – it’s often the result of intense stimulation we endure as an overwhelmed society. From social media to politics, to Covid-19
conversely, the parasympathetic nervous system is associated with the ‘rest and digest state. Fueled by the release of oxytocin, that parasympathetic state is characterized by an intent to bond, connect, share, communicate, and protect. Examples of high oxytocin states include childbirth, nursing, hugging, orgasm, and deep eye contact. Psychedelics such as MDMA, psilocybin, and LSD also markedly increase the release of oxytocin—putting the body into a parasympathetic state that makes it more possible to self-repair. MDMA also promotes reduced activity in the left amygdala helping people access otherwise painful memories without triggering habitual fear responses. This dual effect is largely what makes MDMA so effective in treating PTSD.
Bringing it All Together
So let’s bring it all together. By boosting serotonin, stimulating the production of BDNF, and increasing the transmission of glutamate, psychedelics help heighten the connectivity between neurons—making it easier for people to learn, think creatively, and imagine new ways of being. By quieting down the DMN, they simultaneously allow people to observe their deepest thoughts and emotions without triggering trauma responses. Within this deep state of neuroplasticity, it becomes possible to retrain our neural patterns, making it easier to adopt new behaviors.

At the same time, psychedelics help to reduce inflammation in both the body and brain, which can help to enhance mood, augment cognition, and empower people to better process their emotions. By allowing people to drop into a parasympathetic state, it also becomes possible for the body to heal and for the mind to release anxiety. As a bonus, the parasympathetic state makes people more open to forging meaningful connections.

